CANCER also known as a malignant tumour or malignant neoplasm, is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. Not all tumours are cancerous; benign tumours do not spread to other parts of the body. Possible signs and symptoms include: a new lump, abnormal bleeding, a prolonged cough, unexplained weight loss, and a change in bowel movements among others. While these symptoms may indicate cancer, they may also occur due to other issues. There are over 100 different known cancers that affect humans.

Tobacco use is the cause of about 22% of cancer deaths. Another 10% is due to obesity, a poor diet, lack of physical activity, and consumption of alcohol. Other factors include certain infections, exposure to ionizing radiation, and environmental pollutants. In the developing world nearly 20% of cancers are due to infections such as hepatitis B, hepatitis C, and human papillomavirus (HPV). These factors act, at least partly, by changing the genes of a cell. Typically many such genetic changes are required before cancer develops. Approximately 5–10% of cancers are due to genetic defects inherited from a person’s parents. Cancer can be detected by certain signs and symptoms or screening tests. It is then typically further investigated by medical imaging and confirmed by biopsy.
Many cancers can be prevented by not smoking, maintaining a healthy weight, not drinking too much alcohol, eating plenty of vegetables, fruits and whole grains, being vaccinated against certain infectious diseases, not eating too much processed and red meat, and avoiding too much exposure to sunlight. Early detection through screening is useful for cervical and colorectal cancer. The benefits of screening in breast cancer are controversial. The chance of survival depends on the type of cancer and extent of disease at the start of treatment. In children under 15 at diagnosis the five-year survival rate in the developed world is on average 80%.
In 2012 about 14.1 million new cases of cancer occurred globally (not including skin cancer other than melanoma). It caused about 8.2 million deaths or 14.6% of all human deaths. The most common types of cancer in males are lung cancer, prostate cancer, colorectal cancer, and stomach cancer, and in females, the most common types are breast cancer, colorectal cancer, lung cancer, and cervical cancer. If skin cancer other than melanoma were included in total new cancers each year it would account for around 40% of cases. In children, acute lymphoblastic leukaemia and brain tumours are most common except in Africa where non-Hodgkin lymphoma occurs more often. In 2012, about 165,000 children under 15 years of age were diagnosed with cancer. The risk of cancer increases significantly with age and many cancers occur more commonly in developed countries. Rates are increasing as more people live to an old age and as lifestyle changes occur in the developing world
Definitions
Cancers are a large family of diseases that involve abnormal cell growth with the potential to invade or spread to other parts of the body. They form a subset of neoplasms. A neoplasm or tumour is a group of cells that have undergone unregulated growth, and will often form a mass or lump, but may be distributed diffusely.
All tumour cells show the six hallmarks of cancer. These are characteristics that the cancer cells need to produce a malignant tumour. They include:
- Cell growth and division without the proper signals to do so
- Continuous growth and division even when there are signals telling them to stop
- Avoidance of programmed cell death
- Limitless number of cell divisions
- Promoting blood vessel construction
- Invasion of tissue and formation of metastases
The progression from normal cells to cells that can form a detectable mass to outright cancer involves multiple steps known as malignant progression.
Signs and symptoms
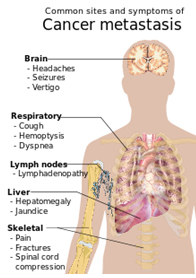
Symptoms of cancer metastas is depend on the location of the tumour.
When cancer begins, it invariably produces no symptoms. Signs and symptoms only appear as the mass continues to grow or ulcerates. The findings that result depend on the type and location of the cancer. Few symptoms are specific, with many of them also frequently occurring in individuals who have other conditions. Cancer is the new “great imitator”. Thus, it is not uncommon for people diagnosed with cancer to have been treated for other diseases, which were assumed to be causing their symptoms.
Systemic symptoms
General symptoms occur due to distant effects of the cancer that are not related to direct or metastatic spread. These may include: unintentional weight loss, fever, being excessively tired, and changes to the skin. Hodgkin disease, leukaemia’s, and cancers of the liver or kidney can cause a persistent fever of unknown origin. Some cancers may cause specific groups of systemic symptoms, termed Para neoplastic phenomena. Examples include the appearance of myasthenia gravis in thymoma and clubbing in lung cancer.
Causes
The great majority of cancers, some 90–95% of cases, are due to environmental factors. The remaining 5–10% are due to inherited genetics. Environmental, as used by cancer researchers, means any cause that is not inherited genetically, such as lifestyle, economic and behavioural factors, and not merely pollution. Common environmental factors that contribute to cancer death include tobacco (25–30%), diet and obesity(30–35%), infections (15–20%), radiation (both ionizing and non-ionizing, up to 10%), stress, lack of physical activity, and environmental pollutants.
It is nearly impossible to prove what caused a cancer in any individual, because most cancers have multiple possible causes. For example, if a person who uses tobacco heavily develops lung cancer, then it was probably caused by the tobacco use, but since everyone has a small chance of developing lung cancer as a result of air pollution or radiation, then there is a small chance that the cancer developed because of air pollution or radiation. Excepting the rare transmissions that occur with pregnancies and only a marginal few organ donors, cancer is generally not a transmissible disease.
Chemicals
Alcohol and cancer and Smoking and cancer
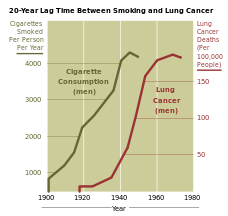
The incidence of lung cancer is highly correlated with smoking.
Exposure to particular substances have been linked to specific types of cancer. These substances are called carcinogens. Tobacco smoking, for example, causes 90% of lung cancer. It also causes cancer in the larynx, head, neck, stomach, bladder, kidney, esophagus and pancreas. Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons. Tobacco is responsible for about one in three of all cancer deaths in the developed world, and about one in five worldwide. Lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently, decreases in smoking rates since the 1950s followed by decreases in lung cancer death rates in men since 1990.
Infection
Infectious causes of cancer
Worldwide approximately 18% of cancer deaths are related to infectious diseases. This proportion varies in different regions of the world from a high of 25% in Africa to less than 10% in the developed world. Viruses are the usual infectious agents that cause cancer but cancer bacteria and parasites may also have an effect.
A virus that can cause cancer is called an oncovirus. These include human papillomavirus (cervical carcinoma), Epstein–Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma), Kaposi’s sarcoma herpesvirus (Kaposi’s sarcoma and primary effusion lymphomas), hepatitis B and hepatitis C viruses (hepatocellular carcinoma), and human T-cell leukemia virus-1 (T-cell leukemias). Bacterial infection may also increase the risk of cancer, as seen in Helicobacter pylori-induced gastric carcinoma. Parasitic infections strongly associated with cancer include Schistosoma haematobium (squamous cell carcinoma of the bladder) and the liver flukes.
Heredity
Cancer syndrome
The vast majority of cancers are non-hereditary (“sporadic cancers”). Hereditary cancers are primarily caused by an inherited genetic defect. Less than 0.3% of the population are carriers of a genetic mutation that has a large effect on cancer risk and these cause less than 3–10% of all cancer. Some of these syndromes include: certain inherited mutations in the genes BRCA1 and BRCA2 with a more than 75% risk of breast cancer and ovarian cancer, and hereditary non polyposis colorectal cancer (HNPCC or Lynch syndrome), which is present in about 3% of people with colorectal cancer, among others.
Hormones
Some hormones play a role in the development of cancer by promoting cell proliferation. Insulin-like growth factors and their binding proteins play a key role in cancer cell proliferation, differentiation and apoptosis, suggesting possible involvement in carcinogenesis.
Hormones are important agents in sex-related cancers, such as cancer of the breast, endometrium, prostate, ovary, and testis, and also of thyroid cancer and bone cancer. For example, the daughters of women who have breast cancer have significantly higher levels of estrogenic and progesterone than the daughters of women without breast cancer. These higher hormone levels may explain why these women have higher risk of breast cancer, even in the absence of a breast-cancer gene.
Diagnosis
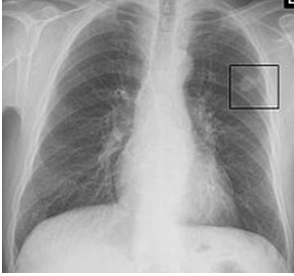
Chest x-ray showing lung cancer in the left lung. Most cancers are initially recognized either because of the appearance of signs or symptoms or through screening. Neither of these lead to a definitive diagnosis, which requires the examination of a tissue sample by a pathologist. People with suspected cancer are investigated with medical tests. These commonly include blood tests, X-rays, CT scans and endoscopy.
Classification
Cancers are classified by the type of cell that the tumour cells resemble and is therefore presumed to be the origin of the tumour. These types include:
Carcinoma: Cancers derived from epithelial cells. This group includes many of the most common cancers, particularly in the aged, and include nearly all those developing in the breast, prostate, lung, pancreas, and colon.
Sarcoma: Cancers arising from connective tissue (i.e. bone, cartilage, fat, nerve), each of which develops from cells originating in mesenchyme cells outside the bone marrow.
Lymphoma and leukemia: These two classes of cancer arise from hematopoietic (blood-forming) cells that leave the marrow and tend to mature in the lymph nodes and blood, respectively. Leukaemia is the most common type of cancer in children accounting for about 30%.
Germ cell tumor: Cancers derived from pluripotent cells, most often presenting in the testicle or the ovary (seminoma and dysgerminoma, respectively).
Blastoma: Cancers derived from immature “precursor” cells or embryonic tissue. Blastomas are more common in children than in older adults.
Prevention
Cancer prevention is defined as active measures to decrease the risk of cancer. The vast majority of cancer cases are due to environmental risk factors, and many, but not all, of these environmental factors are controllable lifestyle choices. Thus, cancer is considered a largely preventable disease. Between 70% and 90% of common cancers are due to environmental factors and therefore possibly preventable.
Greater than 30% of cancer deaths could be prevented by avoiding risk factors including: tobacco, overweight / obesity, an insufficient diet, physical inactivity, alcohol, sexually transmitted infections, and air pollution. Not all environmental causes are controllable, such as naturally occurring background radiation, and other cases of cancer are caused through hereditary genetic disorders, and thus it is not possible to prevent all cases of cancer.
Medication
Vitamins have not been found to be effective at preventing cancer, although low blood levels of vitamin D are correlated with increased cancer risk. Whether this relationship is causal and vitamin D supplementation is protective is not determined. Beta-Carotene supplementation has been found to increase lung cancer rates in those who are high risk. Folic acid supplementation has not been found effective in preventing colon cancer and may increase colon polyps. It is unclear if selenium supplementation has an effect.
Vaccination
Vaccines have been developed that prevent infection by some carcinogenic viruses. Human papillomavirus vaccine (Gardasil and Cervarix) decreases the risk of developing cervical cancer. The hepatitis B vaccine prevents infection with hepatitis B virus and thus decreases the risk of liver cancer. The administration of human papillomavirus and hepatitis B vaccinations is recommended when resources allow.
Screening
Unlike diagnosis efforts prompted by symptoms and medical signs, cancer screening involves efforts to detect cancer after it has formed, but before any noticeable symptoms appear. This may involve physical examination, blood or urine tests, or medical imaging.
Cancer screening is currently not possible for many types of cancers, and even when tests are available, they may not be recommended for everyone. Universal screening or mass screening involves screening everyone. Selective screening identifies people who are known to be at higher risk of developing cancer, such as people with a family history of cancer. Several factors are considered to determine whether the benefits of screening outweigh the risks and the costs of screening. These factors include:
- Possible harms from the screening test: for example, X-ray images involve exposure to potentially harmful ionizing radiation.
- The likelihood of the test correctly identifying cancer.
- Possible harms from follow-up procedures.
- Whether suitable treatment is available.
- Whether early detection improves treatment outcomes.
- Whether the cancer will ever need treatment.
- Whether the test is acceptable to the people: If a screening test is too burdensome (for example, being extremely painful), then people will refuse to participate.
- Cost of the test.
Chemotherapy
Chemotherapy is the treatment of cancer with one or more cytotoxic anti-neoplastic drugs (chemotherapeutic agents) as part of a standardized regimen. The term encompasses any of a large variety of different anticancer drugs, which are divided into broad categories such as alkylating agents and antimetabolites. Traditional chemotherapeutic agents act by killing cells that divide rapidly, one of the main properties of most cancer cells.
Chemotherapy is the treatment of cancer with one or more cytotoxic anti-neoplastic drugs (chemotherapeutic agents) as part of a standardized regimen. The term encompasses any of a large variety of different anticancer drugs, which are divided into broad categories such as alkylating agents and antimetabolites. Traditional chemotherapeutic agents act by killing cells that divide rapidly, one of the main properties of most cancer cells.
Radiation
Radiation therapy involves the use of ionizing radiation in an attempt to either cure or improve the symptoms of cancer. It works by damaging the DNA of cancerous tissue leading to cellular death. To spare normal tissues (such as skin or organs, which radiation must pass through to treat the tumor), shaped radiation beams are aimed from several angles of exposure to intersect at the tumor, providing a much larger absorbed dose there than in the surrounding, healthy tissue. As with chemotherapy, different cancers respond differently to radiation therapy.
Radiation therapy is used in about half of all cases and the radiation can be from either internal sources in the form of brachytherapy or external radiation sources. The radiation is most commonly low energy x-rays for treating skin cancers while higher energy x-ray beams are used in the treatment of cancers within the body. Radiation is typically used in addition to surgery and or chemotherapy but for certain types of cancer, such as early head and neck cancer, may be used alone. For painful bone metastasis, it has been found to be effective in about 70% of people.
Surgery
Surgery is the primary method of treatment of most isolated solid cancers and may play a role in palliation and prolongation of survival. It is typically an important part of making the definitive diagnosis and staging the tumour as biopsies are usually required. In localized cancer surgery typically attempts to remove the entire mass along with, in certain cases, the lymph nodes in the area. For some types of cancer this is all that is needed to eliminate the cancer.
Palliative care
Palliative care refers to treatment that attempts to make the person feel better and may or may not be combined with an attempt to treat the cancer. Palliative care includes action to reduce the physical, emotional, spiritual, and psycho-social distress experienced by people with cancer. Unlike treatment that is aimed at directly killing cancer cells, the primary goal of palliative care is to improve the person’s quality of life.

People at all stages of cancer treatment should have some kind of palliative care to provide comfort. In some cases, medical specialty professional organizations recommend that people and physicians respond to cancer only with palliative care and not with cure-directed therapy. This includes:
- people with low performance status, corresponding with limited ability to care for themselves
- people who received no benefit from prior evidence-based treatments
- people who are not eligible to participate in any appropriate clinical trial
- people for whom the physician sees no strong evidence that treatment would be effective
Palliative care is often confused with hospice and therefore only involved when people approach end of life. Like hospice care, palliative care attempts to help the person cope with the immediate needs and to increase the person’s comfort. Unlike hospice care, palliative care does not require people to stop treatment aimed at prolonging their lives or curing the cancer.
Multiple national medical guidelines recommend early palliative care for people whose cancer has produced distressing symptoms (pain, shortness of breath, fatigue, nausea) or who need help coping with their illness. In people who have metastatic disease when first diagnosed, oncologists should consider a palliative care consult immediately. Additionally, an oncologist should consider a palliative care consult in any person they feel has less than 12 months of life even if continuing aggressive treatment.
